
Monica’s daughter, Vera, passing time in the emergency department
My daughter Vera has been fighting acute lymphoblastic leukemia for almost 2 years, and we recently visited the emergency department (ED) after managing to avoid it for 6 months. Going into this last visit, I remembered all the tips an oncology family should know before heading to the ED. I want to call out that most of these tips were learned by experience and/or told to me by a fellow oncology mom. These are things I wish I had known since diagnosis day.
- Always have an ED bag packed full of the essentials. Same mentality as when going into labor and having that hospital bag ready by the door. You just never know when a temperature check becomes a fever or when you need urgent help with symptom management.
- Before heading into the ED, notify your child’s care team so they alert the ED that you are coming, this can help ensure the proper care and expedite wait times.
- Even if you don’t think your child’s port is going to be accessed, follow your child’s normal pre-access care in the event it does happen (numbing cream, bring buzzy bee, and/or cold spray).
- Upon ED arrival, let check-in staff know your child is a pediatric oncology patient, immunocompromised, and you’d like to wait in a private waiting area for their safety. The last thing you want is your already vulnerable child to catch a virus that is running rampant in the ED.

Monica and Vera waiting for their turn in the emergency department
- Before your child’s port is accessed, ask the ED staff when’s the last time they accessed a pediatric patient’s port and are they comfortable doing so. Listen to your gut! If you feel any doubt, request they call the Pediatric Oncology ward for a trained nurse to do the access. In my experience, both parties have always been willing and honestly relieved. There is nothing worse than adding trauma to your child’s ED visit by getting an inexperienced nurse to access their port and it takes several tries.
- Know your child’s port access needle size. This will expedite port access, as ED staff don’t have time to look up your child’s need size, they likely don’t have it handy, and they can call to the pediatric oncology ward to have it sent over.
- In the same notion, know your child’s NG tube size if you are coming back to get it replaced. Placing an NG tube is traumatic for everyone, but it can be even more traumatic if not done with the correct size tube, leading to more discomfort.
- Bring your child’s medications. Being in the ED could be a LONG day! You do not want to miss your child’s timed meds because you thought you’d be out of there in time.
- Speaking of a long day; bring snacks, electronic chargers, dress comfy, bring tablets, books, and other boredom busters to help pass the time and make an anxious environment less so.
- ED staff are meant to help troubleshoot when it comes to their role in a pediatric oncology child’s journey. While they are medically trained professionals, they are not an expert on your child’s diagnosis. That is not their job. Always run ED staff’s guidance and advice by your team. Ask them to connect with your child’s care team. And if desperate times call for desperate measures, call your on-call Onc and put them on speaker phone with the ED physician so you can collaborate on the best next steps for your child.
- If you are lucky to not be admitted and get discharged from the ED, ALWAYS be sure that upon de-access of your child’s central line they flush with heparin. Because the ED staff are not trained as extensively on central line care, they are less privy to flushing with heparin versus saline. Saline is to flush fluids; Heparin helps to keep blood flowing smoothly and from clotting in the catheter, which is essential for functionality and infection prevention.
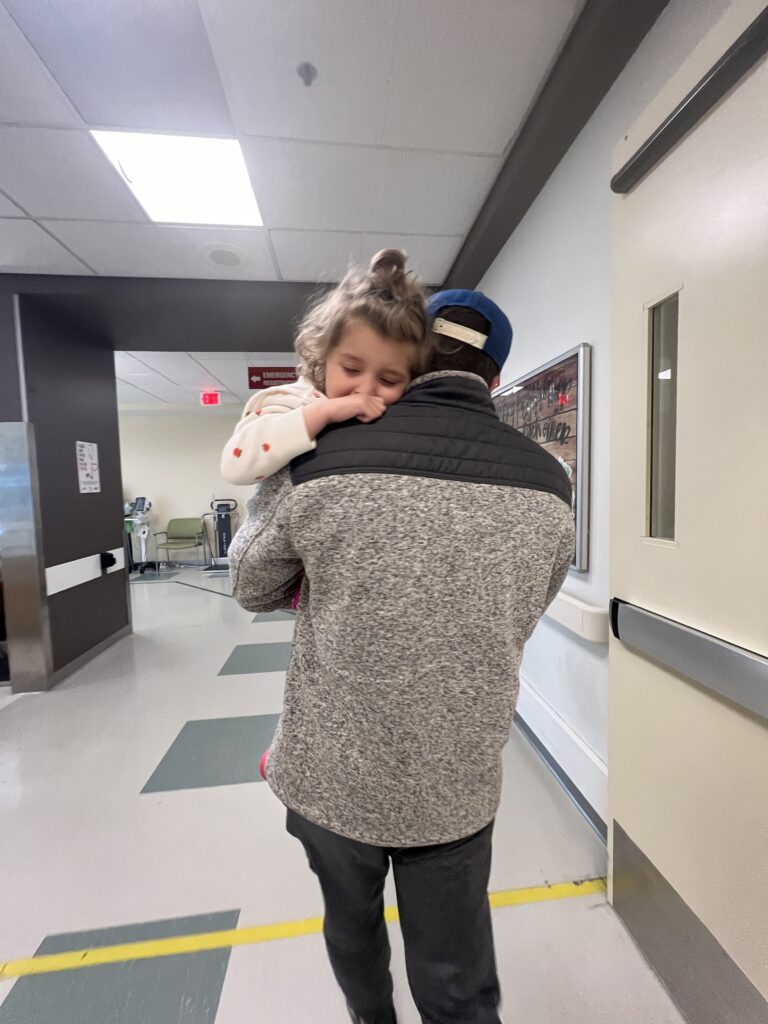
Vera being held by dad in the emergency department
Remember that you are the expert on your child. Sometimes, the ED requires extra advocacy so mentally prepare yourself for over education on your child and have patience with the staff. They have your child’s best interest in mind, but they are not your child’s care team and are doing the best they can with the knowledge they have on your child (which is the spark notes version of your child’s medical history via charts, oncology emails, and your dialogue).
This advice was provided to me from pediatric oncology mamas from all around the country. See their Instagram profiles to follow their journeys, some are in-the-fight, navigating survivorship, and bereaved: Lindsay, Jenny, Helen, Taylor, Carolina, and Cassie.
Donate now and help support research into better treatments for kids with cancer.
Read more on the St. Baldrick’s blog:

 SBF
Tweets »
SBF
Tweets »