About 10 years ago, the St. Baldrick’s Foundation expanded its research portfolio to include funding for supportive care grants. Since then, it has funded more than 40 innovative studies in this area. Supportive care, according to the National Cancer Institute, refers to care given to improve the quality of life of patients who have a serious or life-threatening disease.
Our supportive care grants have encompassed a wide variety of topics, including studies focused on psychosocial screening, survivors’ nutrition and physical activity, chemotherapy-induced neuropathy, and mindfulness training — just to name a few. These grants are in sync with needs across the spectrum of cancer in children and adolescents/young adults (AYA) from diagnosis through active treatment to post-treatment survivorship and life-long health surveillance. As many have said, the cancer experience doesn’t end when treatment ends. Supportive care can improve the quality of life for its entire duration.
For this National Hospice and Palliative Care Awareness Month, we’ve decided to look at some of the reasons why this category of care is so very important to pediatric cancer.
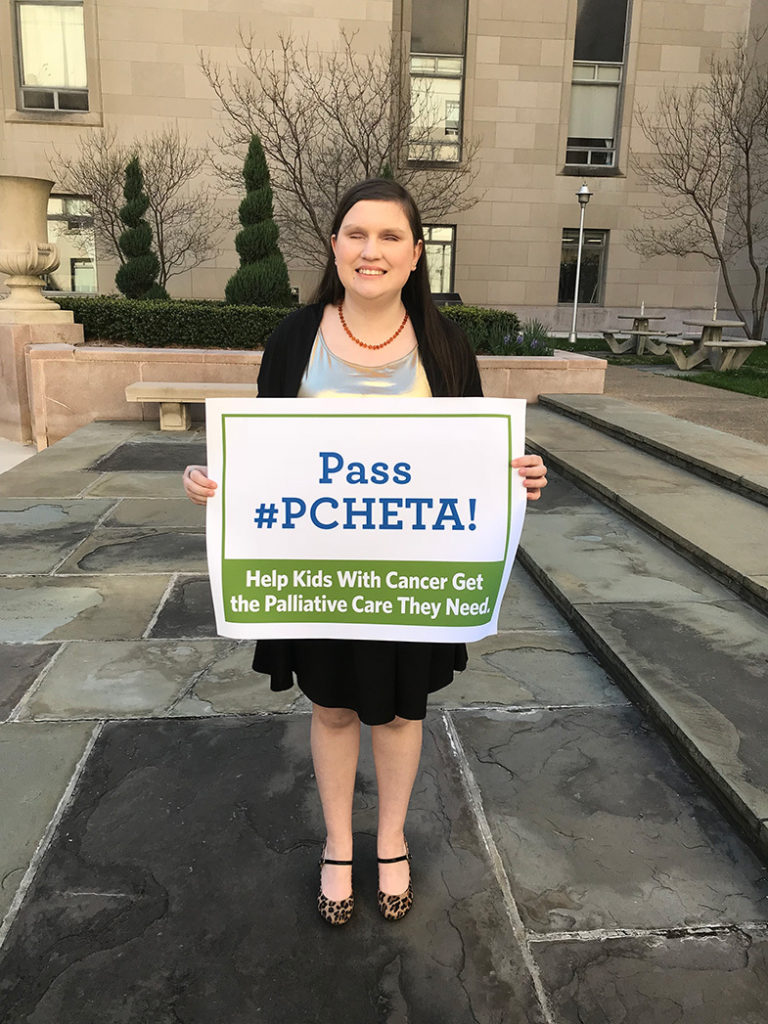 Honored Kid, Tacey, showing her support for PCHETA, at the 2019 Action Days in Washington, D.C..
Honored Kid, Tacey, showing her support for PCHETA, at the 2019 Action Days in Washington, D.C..
Supportive Care Vs. Palliative Care
Supportive care is a broad concept that embraces palliative care, so much so that these terms are often used interchangeably. For more precision, the National Institute of Nursing Research defines pediatric palliative care as “care that eases children’s symptoms of the illness, provides emotional and social support, maintains open communication between all healthcare providers, and helps to initiate discussions about treatment and care options for the child.” Although palliative care can offer an added layer of support for patients and families, its possible benefits can go unrecognized or untapped, partly because of some pervasive myths. In a recent interview with Kathy Ruccione, PhD, RN, MPH, FAAN, and Associate Professor, Department of Doctoral Programs, Azusa Pacific University School of Nursing, she noted that, “Probably the most prominent myth is that palliative care is only for people at the end of life. In fact, the truth is that palliative care can be most effective if it’s integrated soon after diagnosis, so that symptoms can be relieved and suffering can be lessened from the very beginning of the cancer experience. Palliative care is in addition to — not instead of.”
According to Dr. Ruccione, “Sometimes, people may react with distress to a recommendation to begin palliative care because they think they’re being told that death is imminent. In actuality, palliative care can be offered at any point along the continuum of care, but hospice care is specialty care usually offered at the end stage of disease.”
 Kathy Ruccione, PhD, RN, MPH, FAAN, and Associate Professor, Department of Doctoral Programs, Azusa Pacific University School of Nursing
Kathy Ruccione, PhD, RN, MPH, FAAN, and Associate Professor, Department of Doctoral Programs, Azusa Pacific University School of Nursing
The Education Challenge Behind Palliative Care
Of course, patients and their families can’t be accurately informed about palliative care services if their health care professionals themselves aren’t well informed about palliative care. For too long, palliative care has not been adequately covered in health care professionals’ prelicensure training. That’s unfortunate across the health care professions that make up palliative care teams. For example, studies suggest that providing pediatric palliative care education in nursing programs can build nurses’ confidence and better prepare them to competently care for patients and families [1]. For health care professionals to be palliative care myth-busters, they need a rock-solid educational foundation.
PCHETA Makes Its Way Through Congress
To that end, a bill that was passed by the House of Representatives in October, and next moves to the Senate for consideration, the Palliative Care and Hospice Education and Training Act, aims to better prepare health care professionals to provide care for patients and families faced with serious or life-threatening illness. The PCHETA bill would provide funding for additional training for physicians, nurses, pharmacists, social workers and other allied health professionals, along with support for research and programs to increase public awareness of palliative care services. Elements of the bill include:
- Palliative Care and Hospice Education Centers: Establishes centers to improve training for interprofessional healthcare workers in palliative care
- Workforce Development: Creates fellowship programs to provide short-term intensive courses focused on palliative care
- Career Incentive Awards: Provides grants or contracts to teach or practice in the field of palliative care for at least five years
- Nurse Training: Creates special preferences in existing nurse education law for hospice and palliative nursing, in education, practice, and quality grants, workforce development, and nurse retention projects
- Palliative Care Education and Awareness: Provides for a national campaign to inform patients, families and health professionals about the benefits of palliative care
- Enhanced Research: Directs the National Institutes of Health to use existing authorities and funds to expand palliative care research
St. Baldrick’s has been in the forefront of advocating for this legislation. As Dr. Ruccione says, “Reducing suffering and enabling the best possible quality of life for young people with cancer is exactly what supportive care is all about. And that’s something we can all appreciate, whether we’re researchers, clinicians, or young people and their families faced with cancer.”
To learn more about how donations to St. Baldrick’s support the work of Dr. Ruccione and others like her, visit our Research Priorities page, join our Speak Up network, or donate today to fund better treatments and quality of life for kids and help #DFYchildhoodCancers
[1] Negrete, T.N. & Tariman, J.D. (2019). Pediatric palliative care: A literature review of best practices in oncology nursing education programs. Clin J Oncol Nurs 23(6):565-568. doi: 10.1188/19.CJON.565-568
Join us today and help us #DFYchildhoodCancers!
Read more on the St. Baldrick’s blog:

 SBF
Tweets »
SBF
Tweets »